Myoclonus is defined as a sudden onset jerking motion. How is this different from a tremor? Tremors tend to have a creshendo, decreshendo appearance where as myoclonus has been described as "square form" impulse with sudden, rapid onset, sustained contraction, and sudden stop. Okay, fine, it's not a tremor. How do I diagnose myoclonus?
There are four common types:
1) Physiologic - the classic example is hiccups.
2) Epileptic- occur with or around epileptic seizures
3) Idiopathic - unknown origin or cause (rare in veterinary medicine...or we're just missing it.)
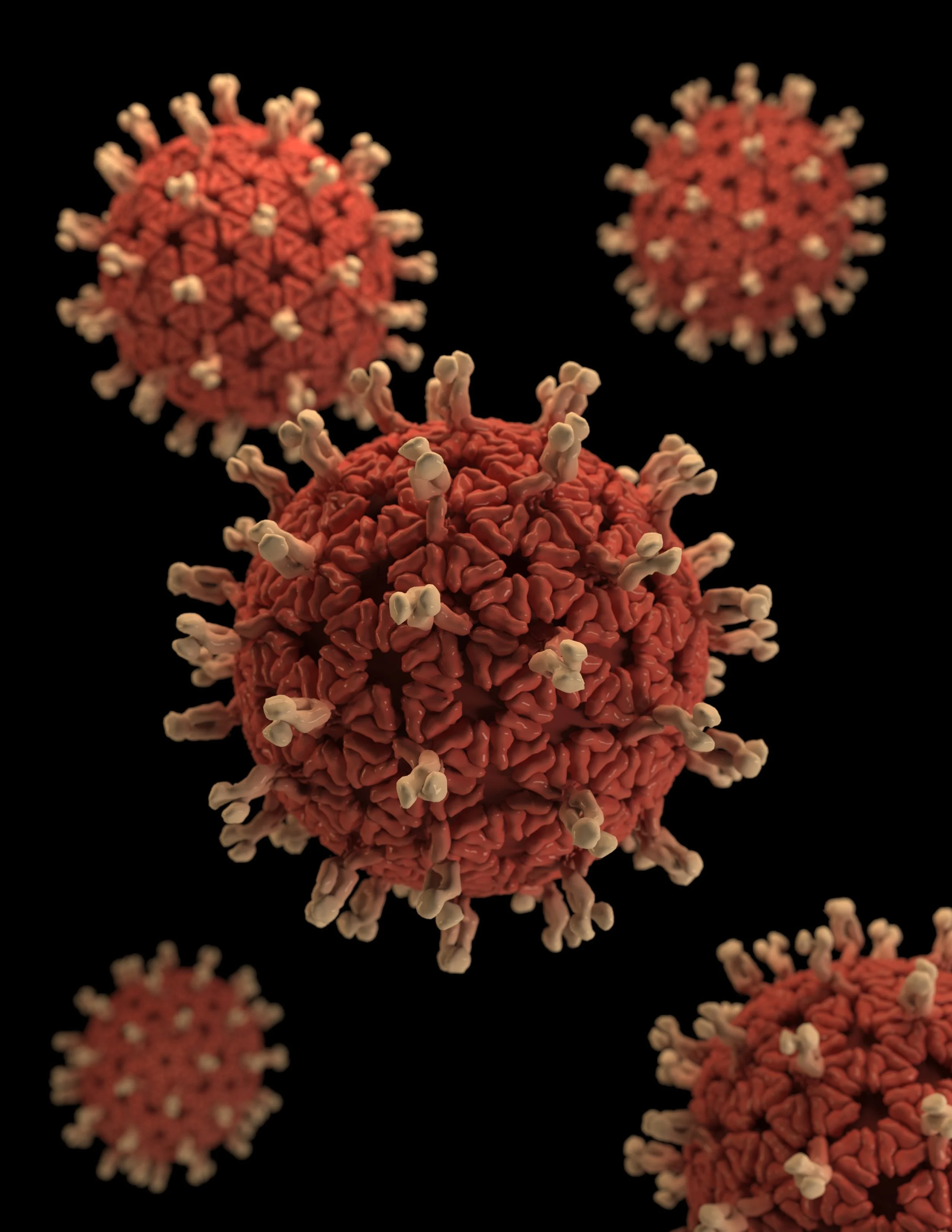
4) Symptomatic - due to an underlying pathology. For example, distemper virus.
Neuroanatomic lesion localization:
1) Cortical - usually associated with myoclonic seizures.
2) Subcortical (brainstem) - "falling asleep" myotonia. In this case, people or animals will suddenly "jerk" just as they fall asleep. Classically, this has been thought to occur because the cortical functions "turn off" before the brainstem functions but this may not be the complete story.
3) Peripheral - an example is hemifacial spasms, or ocular spasms (have you ever had your eyelid twitch annoyingly and you cannot stop it?)
Veterinary neurologists are often consulted for symptomatic and epileptic myoclonus. Although there is a population with idiopathic myoclonus, it is rare. Symptomatic myoclonus occurs at rest, asleep, or during motion. Symptomatic myoclonus does not stop with sleep! The animal may appear aware or unaware of the twitch. If the contraction is happening in a body part used for walking or eating it may be life limiting. If not, animals may live with a myoclonus with minimal disruption. Epileptic myoclonus occurs around a time of seizure activity and is therefore often managed with anticonvulsant management.
Distemper virus is a common cause of canine myoclonus and CNS infections (various causes) have been cited as causes of feline myoclonus. There is no treatment available for distemper virus therefore, patients are monitored for progressive neurologic signs (mentation changes, gait changes, seizures, other) and euthanized if signs are progressive. If the signs are not progressive, usually myoclonus is not a reason for euthanasia.
That's all I have for you today! I hope you enjoyed this TidBit about myoclonus and feel better prepared when you see it in your exam room. :)
Thank you for reading! May you have a wonderful, twitch-free holiday week!
Neuroanatomic Lesion Localization Practice book!
It's Here! The Small Animal Neuroanatomic Lesion Localization Practice Book by yours truly!
It's always hard to self promote, so instead I wish to draw your attention to the many neurologists that contributed cases that made this little workbook the workhorse that it is.
1. Dr. Helena Rylander (UW-VC neurologist)
2. Dr. Joy Delamaide-Gasper (MVS neurologist)
3. Dr. Kari Foss (U of I neurologist, and former student)
4. Dr. Devon Hague (U of I neurologist)
5. Dr. Julien Guevar (Swiss neurologist and former UW-VC Neurologist)
6. Dr. Susan Arnold (U of Minnesota Neurologist and UW- VC graduate)
7. Dr. Sam Long (Australian neurologist and all around amazing guy)
8. Dr. Simon Platt (Forum UGA neurologist and ACVIM-Neurology past president)
The Small Animal Neuroanatomic Lesion Localization Practice Book is just that - a practice book - geared for general practitioners, students, and interns who are interested in brushing up or dusting off their neuroanatomic lesion localization skills. This little ditty has 7 chapters, with many cases in each chapter for you to try your hand at neuroanatomic lesion localization.
Not enticed enough?? If you get stuck - you know the author of the book and can email me directly for help! (yay for connections!)
Still not enticed?? Check out this link to see more: https://www.cabidigitallibrary.org/doi/10.1079/9781789247947.0000
Cost $65 USD
Note: I don't get any notifications of who buys a book, but if you suddenly stop consulting I'll assume you bought the book and learned it all and no longer need me. I really should stop trying to teach myself out of a job.... :)
That's it for this week. Not a typical TidBit per se, but hopefully you don't mind so much. Thanks for reading!
Have a great week!
Bruxism and Forebrain Disease
Bruxism is defined, in human medicine, as repetitive, involuntary, masticatory muscle activity, often appears as grinding teeth, bracing or thrusting of the mandible. There are two types: awake and asleep. Asleep bruxism is quite commonly reported in humans and can be triggered by stress or anxiety. Awake bruxism, or uncontrolled bruxism during awake states, is a very different thing. Awake bruxism (AB) can be broken into pathologic or physiologic causes. Physiologic causes don't apply to veterinary medicine so let's dig deeper into pathologic, awake bruxism. Within the pathologic group there are idiopathic causes and symptomatic causes. Neurologic diseases such as inflammatory conditions, traumatic or congenital disease, epilepsy and a host of other causes have been reported to be associated with awake bruxism in humans. A recent article, published in the JVIM, noted that bruxism secondary to a neurologic cause is most commonly awake bruxism.
Have you seen a dog with Bruxism? The recent article by Liatis T, et al, evaluated AB in 4 dogs over a span of 11 years so don't feel badly if you've not seen one! A link to the entire report is found at the bottom. Although previously reported in dogs with congenital storage disorders, it is rare in mature adult dogs. In this study, two dogs were presented by the owners with a complaint of AB, along with other clinical signs of neurologic disease. AB was noted in the second two dogs by the attending clinicians during evaluation. AB was episodic in all four dogs, occurring throughout the day and always stopped when distracted. No post ictal signs were noted and no autonomic signs were seen during or after the event. All four dogs had forebrain lesions!
Take away: If you evaluate a dog for awake bruxism, or if you note it during the exam while evaluating the pet for other neurologic abnormalities, consider it abnormal. It is not pathognomonic for forebrain disease but, at least according to this report, is strongly supportive of a forebrain lesion. This may be an indication to get a neurology consultation and advanced imaging.
Link: https://onlinelibrary.wiley.com/doi/full/10.1111/jvim.16570?campaign=wolearlyview
Thanks for reading! I look forward to working with you again soon.
Exercise and Seizure Control
Last year we talked about a temporal relationship between seizures and exercise. It has been shown that seizures rarely occur DURING exercise.
Recently, I was involved in a study, performed at the University of Wisconsin, evaluating increased activity and it's relationship to seizure development. In this study, dogs were tracked using a FitBark(tm) exercise tracker for 3 months and then prescribed a 20% increase in activity over the next 3 months. Seizure frequency and "seizure days' (the number of days that a dog has a seizure) per month were evaluated. Unfortunately, many of the dogs did not actually do the exercise increase as prescribed (ugh!) but even accounting for that, exercise was not associated with a statistically significant reduced seizure frequency or number of seizure days during the study period.
Why didn't this work? There are many possible reasons why prescribed exercise didn't change the seizure frequency. The most obvious reason is that not enough pets made the change to show a statistical difference. The other, more concerning option, is that exercise really doesn't have an effect on overall seizure performance. There are mixed results in the human epilepsy studies. Although it is rare to have seizures during activity, it can happen. Furthermore, some studies showed a lower seizure frequency when exercise was added to a treatment plan and other studies did not.
What is the take home message? Increased activity cannot (yet) be used as an adjunctive treatment for seizure management. It is still a healthy choice, and should be encouraged in all pets but especially our dogs with epilepsy but not, sadly, as a means to seizure control. This was a small study, so my hope is that future studies will yield more robust results.
Thanks for reading! If you want to read the whole study you can find it here: https://onlinelibrary.wiley.com/doi/epdf/10.1111/jsap.13568
Have a great week. Happy Thanksgiving! Enjoy exercising with your pets, friends, and family this holiday week!
Dogs Fall in the Fall
Today, you're presented with a 4 year old German Short-Haired Pointer with a history of rapidly progressive difficulty walking. Although your heart rate may be going up when you read this on your schedule, you're calm, cool and collected as you pick up your pleximeter and head into the room.
Your technician has provided the following history for you: The pet was out hunting last weekend with the owner and no unusual circumstances occurred. He did run away two days ago and came back with a small bite wound on his muzzle. The pet is up-to-date on vaccination (including rabies) and has not had any change in voiding habits prior to the last 24 hours. The dog is fed a mixture of a commercial kibble diet and raw meat. There is no reported prior medical history.
Physical exam: Unremarkable other than the bite wound. It is healing, not infected (visual inspection only) and does not appear to be bothering him. He is his typical, high strung, friendly self!
Neurologic examination:
Mentation: BAR
Cranial nerves: normal
Postural reactions: Absent in 3 of four limbs, reduced in right front limb only.
Reflexes: Absent patellar reflexes bilaterally, absent withdrawal reflexes in both pelvic limbs (but he howled pitifully when you tried to do it!) reduced withdrawal in both thoracic limbs, more notable on the left thoracic limb than the right. Absent cutaneous trunci reflex to T6 on the left, and reduced to T/L junction on right.
Palpation: non-painful on palpation but hyperesthetic when trying to do reflexes. This is unusual for him as he doesn't typically mind his feet touched or even flinch during vaccinations.
Gait: Non-ambulatory tetraparetic with paraplegic (no motor observed in PL), marked paresis in both thoracic limbs, more noted in left than right.
Neuroanatomic lesion localization:
First, decide if this is brain or spinal cord.
1. Brain: With reduced reflexes, it isn't a brain problem.
2. Spinal cord: It could be a spinal cord problem, but then it must be localized to BOTH C6-T2 and L4-S3 (entire plexi for both sites) and, although possible, it is highly unusual. If that is where we localize the problem, how do we account for the c. trunci reflex? Based on the findings, it should suggest a lesion mid thoracic lesion (1-2 segments cranial to the cranial most reflex) and that doesn't fit in either C6-T2 or L4-S3 segments, does it? No. Therefore, this isn't a spinal cord problem either. This is neuromuscular, my friends!
Neuromuscular neuroanatomic lesion localization.
We can narrow it down further within the neuromuscular localization. You have 3 choices: 1) Muscle 2) neuromuscular junction and 3) nerve. Dogs with myopathies (muscle disease) have normal reflexes (and he doesn't) so it isn't a myopathy. Dogs with disease of the neuromuscular junction have absent reflexes (and he does), so it could be this. Dogs with a peripheral neuropathy often have patchy loss of reflexes (and he does) so it could be this. Therefore, you would suspect either a neuromuscular junctionopathy or peripheral neuropathy in this dog.
Differential diagnoses:
1. Junctionopathy - botulism, tick paralysis, coral snake envenomation, Ca blockers, acute myasthenia gravis (rare).
2. Acute peripheral neuropathy - hypothyroid crisis, polyradiculoneuropathy (APN), autoimmune (rare).
Of these, the most likely is APN (Coonhound paralysis) based on the dog's history, neurologic exam and signalment.
Although an ELISA test does exist (Developed at UW-Vet School), it has a long turn around time and therefore isn't terribly useful for the initial diagnosis. I find it helpful to rule out the other causes rather than focusing on diagnosis this cause. I suggest applying a tick repellant (rule out tick paralysis), submitting a myasthenia titer, checking CBC, serum biochemistry for signs of biochemical imbalance (calcium specifically) and a T4. If all of this is normal, we're likely back to acute polyradiculoneuropathy (APN).
Treatment is purely supportive. This disease is caused by an autoimmune attack against the nerve roots triggered by many things, including racoon saliva. Yes, saliva. Interestingly, a report in 2019 found an association with the consumption of raw meat contaminated with Campylobacter jejunii within 7 days of the development of APN. Antibodies are available and can be administered in the early phase but may not be available in your area. Supportive care includes ventilatory monitoring and mechanical ventilation as needed (they can loose the ability to contract the intercostal muscles and therefore cannot inhale), nutritional support (they can eat, drink and void voluntarily but need to do so sternal and be cleaned frequently to avoid bedsores), and nursing care (see prior). Signs reach peak severity within 10 days for most dogs. Signs typically improve within 3 months (12 weeks). Please note that this disease is very recoverable with appropriate nursing care but it takes long, and intensive, at home nursing care. Sadly, affected dogs do not gain a sustained immunity after they recover and can show signs again if they are exposed to an appropriate trigger.
Please let me know if you have any questions about today's TidBit Tuesday. I hope you have a great week!
Masticatory Muscle Myositis: That's a mouthful!
We are seeing more cases of masticatory muscle myositis lately so I thought we'd look into this interesting diagnosis together. Let's start by defining it.
Masticatory Muscle Myositis (MMM) is an inflammatory, autoimmune myopathy affecting the muscles of mastication (temporalis, masseter, pterygoid and rostral digastricus). All of these muscles are innervated by CN 5, specifically the mandibular branch.
Why only these muscles?
The muscles listed above have a specific myofiber type (type 2M), which is only present in these muscles and some fetal muscles. All other muscles in the body are 1A and 2A fiber types! Therefore, these muscles present a unique antigen for the immune system to target.
What does the clinical picture look like?
There is an acute phase, and a chronic phase. The acute phase occurs first and often includes signs such as jaw pain, swollen muscles, and difficulty chewing. (Note NOT drop jaw or difficulty closing the jaw....that is a different disease.)
If left untreated, patients will then progress into the chronic phase, which includes signs such as muscle atrophy and an inability to open the jaw. Muscle fibers are replaced with scar tissue during the chronic phase making the dog unable to open their mouth more than a few centimeters over time.
Must we take a chunk of muscle to make this diagnosis?
No, you don't! Although you will obtain a diagnosis in both the acute and chronic phase, there is an easier, and less invasive, way. The serum 2M antibody test is both highly sensitive (85-90%) and highly specific (100%) and is the preferred diagnostic test for MMM. Send it to the Comparative Neuromuscular Lab in La Jolla CA (https://vetneuromuscular.ucsd.edu/) if you live in the states. I think there are other choices worldwide but I'm not as aware of those.
Steroids are the best, and most effective treatment.
Immunosuppressive steroids are the most effective treatment for this disease and are strongly recommended in the acute phase. Your goal is to stop that inflammation in its tracks so that the patient doesn't progress to the chronic phase. Once they replace the muscle fibers with connective tissue, the game is over. The dog cannot open its mouth, chew, or be safely intubated or vomit. The chronic stage results in poor quality of life. Steroid protocols vary by neurologist. My protocol starts with 1 mg/kg PO q12h prednisone for 30 days, and then tapers slowly from there. Repeat 2M antibody titers every 1-2 months is recommended. Once the numbers return to normal, it is generally safe to stop the steroid administration.
If any dog has painful muscles of mastication, struggles to open its jaw without pain, and has an elevated CK on lab work a 2M antibody titer is recommended. Don't forget: neospora caninum and toxoplasma gondii can cause myositis and do attack the muscles of mastication. Concurrent testing for these two diseases in all dogs is strongly encouraged before starting immunosuppressive prednisone. I have been taken by surprise how often these tests are positive when I suspect this is "just" MMM.
Hopefully this helps you address muscle pain in your patients. If you have a question about a patient, please contact me via email or schedule a consultation online! Have a great week!
Triggers for MUO
Renal Tubular Acidosis and Zonisamide
Ahh, it is time to examine Zonisamide again. A recent article in Veterinary Medicine and Science described a single dog with lethargy and distal renal tubular acidosis following administration of zonisamide. (https://onlinelibrary.wiley.com/doi/epdf/10.1002/vms3.905)
Distal renal tubular acidosis (RTA) has been defined as a normal anion gap metabolic acidosis with alkaline urine.
What should I look for to diagnose RTA?
The dog in this report had hypochloremia and hyperkalemia on initial blood work. This, coupled with a mild acidosis on blood gas and a urine pH of 7.73, suggested RTA. We're not sure of the consequences of RTA in dogs, yet. In pediatric human epileptic patients, there is some concern for future renal disease with RTA but this hasn't been well established (to my knowledge) for dogs. In this case, the link between the RTA and the dog's clinical lethargy was made, which is what drove the clinicians to pursue treatment.
How is it treated?
The authors described a very slow infusion of bicarbonate (please don't do this unless you have 24 hour monitoring capability!) which reversed the clinical lethargy and normalized the blood gas imbalance for 3 days. They did try to reduce the dose of zonisamide prior to treating the acidosis and achieved mild clinical improvement of sedation when the serum zonisamide concentration went from 38.6 ug/ml to 15.1 ug/ml. No change in biochemical status was noted. If you don't have the option to do a bicarbonate infusion, slowly tapering down or off of zonisamide is recommended to reverse the RTA. It is unknown, in dogs, if sustained RTA has negative health consequences. For many patients, another anticonvulsant drug must be substituted prior to removing zonisamide from the treatment plan.
Another short, but sweet TidBit Tuesday. Please let me know if you have any questions!
I hope those of you here in Wisconsin enjoyed the wonderful weather we had this past weekend and have found your winter hats and gloves in preparation for this coming weekend. Bring it on, am I right??
Cranial Nerve Refresher!
Consensus Statement for Intervertebral Disc Herniation in Dogs, 2022
October, 2022... We have long known that intervertebral disc herniation type I (IVDH) affects chondrodystrophic dogs, at a young age, disproportionately compared to non-chondrodystrophic dogs. We also know that many dogs benefit from surgical and medical intervention. We also know that the neurologic examination is a major predictive factor on recovery (medical and surgical intervention). What we don't know, is how to put what we know into a digestible nugget for clients to hear and understand when in our exam rooms with a dog with suspected IVDH.
First things first... We diagnose IVDH with MRI, CT, CT-myelogram or just myelogram. We don't diagnose IVDH on plain radiographs, or on neurologic exam. (Sorry, soapbox here.) When I say a dog "with IVDH" I mean that they have undergone some sort of diagnostic imaging (MRI, CT, CT-myelography or myelogram) and have been found to have compression to the spinal cord from suspected or confirmed herniated disc material. Presumably, of type I nature for this TidBit. If we don't have diagnostic imaging, but have a chondrodystrophic dog (beagles are included in this group) with appropriate neurologic signs we can call it "presumptive or suspect IVDH". We should, honestly, discuss other differential diagnoses with clients to ensure they understand that there are other possible causes so their decisions are informed. Common diseases that can mimic IVDH could include (but are not limited to) meningomyelitis, neoplasia, Syringohydromyelia, discospondylitis, and spinal trauma/fracture.
Medical intervention... The cornerstone of medical intervention is bedrest for 3+ weeks, anti-inflammatory (typically NSAIDS, but some neurologists prefer steroids), and muscle relaxants or pain management, if the pet is painful. See below for the consensus statement recommendations for medical intervention.
Surgical intervention.... I think this one is self explanatory (mostly). One small point I'll make is that fenestration is not always included when discussing surgical intervention. I consider fenestration an important part of surgical treatment but it does NOT decompress the spinal cord and is therefore excluded in lots of literature. Fenestration means to make a "window" in the affected disc UNDER the spinal canal and remove disc through a lateral or ventral incision (TL vs C-spine). This is also performed in adjacent discs in most cases.
July 2022...ACVIM consensus statement on diagnosis and management of acute canine thoracolumbar intervertebral disc exclusion (doi/epdf/10.1111/jvim.16480). A few key points are listed below and I will have more to share with you in future weeks.
Outcome of dogs managed medically or surgically, based on severity of presenting signs
Pain only. 80% of dogs had positive outcomes with medical management. 98.5% of dogs had positive outcome with surgical management.
Non-ambulatory paraparesis. 81% had positive outcomes with medical management however the level of recovery was less complete with medical management. 93% had positive outcomes with surgical management.
Paraplegia, deep pain intact. 60% of dogs had positive outcomes with medical management however this was prolonged and less complete compared to surgical management. 93% of dogs had positive outcomes with surgical management.
Paraplegia, deep pain absent. 21% of dogs had a positive outcome. 61% of dogs had a positive outcome.
The loss of deep pain causes the biggest shift in predictive statistics for surgical intervention. If you have any question about checking deep pain, please ask!
Medical management key points
Strict rest of 4 weeks is recommended based on low-level evidence to allow for healing of the annulus fibrosus. Strict rest is recommended by all, the 4 weeks part has low-level evidential support in the literature.
Corticosteroids are NOT recommended in acute intervertebral disc herniation and their use did not demonstrate superior outcomes in many studies. The exception is management of chronic signs in which corticosteroid use may show some benefit. (Not addressed in this article.)
NSAID use is recommended for at least 5-7 days, assuming no specific contraindication exists.
There is low-level evidential support for acupuncture or rehabilitation for dogs.
Surgical management key points
Much of the information provided is useful if you perform the surgery. If you do, please seek out the article as I won't be presenting those points here.
The timing of surgical decompression is hotly contested amongst neurologists (and surgeons performing neurosurgery). Conventional wisdom suggests early decompression leads to better long-term outcomes, and faster. This has not been consistently shown in the literature therefore the consensus statement elected to skirt the issue and not provide a "optimal window of time" recommendation. My thoughts (I was not on the consensus team, please note) is that if your client is able to seek surgical management please do so as quickly as possible.
That's it for this week. This is supposed to be a "TidBit" so I don't want to overwhelm you and discourage you from reading. If you perform these surgeries, or refer frequently, please consider reading the consensus statement. If you have any questions about what I've covered so far, or IVDH in general, please reach out! I will cover more from this statement paper in future TidBit Tuesdays!
Have a great week, stay warm, and enjoy these glorious sunny days of fall!
Predictive Signs for MUO
Meningoencephalitis of unknown origin (MUO) is a non-infectious, inflammatory brain disease common in dogs. The vast majority of dogs diagnosed with meningoencephalitis have MUE, not infectious meningitis. MUO includes granulomatous meningoencephalitis (GME) and the necrotizing encephalitides (NME,NLE) and is the term used to describe antemortem non-infectious, inflammatory CNS diseases in dogs and cats. Providing owners with a prognosis when diagnosed with MUO is extremely challenging. A recent study evaluated several prognostic factors on the early survival in dogs with MUO. (https://www.sciencedirect.com/science/article/abs/pii/S1090023322000995)
Key Points:
98 dogs with MUO were included. 30/98 died within 30 days of the diagnosis.
Adding cytosar to a glucocorticoid protocol did NOT alter the prognosis.
Obtundation at presentation was the ONLY factor statistically associated with poor prognosis. Dogs had a 6.6x higher odds of death in the first 7 days, 2.1x increased risk in the first 30 days when presenting with obtunded mentation.
What does this mean for your patients?
It means that we still have a long way to go when sorting out what MUO means, and how it affects dogs. It means that a dog with a severely elevated WBC on CSF, or with other abnormalities on neurologic examination do not necessarily have a poorer prognosis. If you are seeing a patient with multifocal CNS neuroanatomic lesion localization, be sure to evaluate the pet's level of mentation. Survival may be reduced if obtundation is present. Refer as soon as possible for a neurology consultation and/or work up, depending on client preferences.
References: Lawn RW, Harcourt-Brown TR. Risk factors for early death or euthanasia within 100 days of diagnosis in dogs with meningoencephalitis of unkonwn origin. Vet J 2022. vol. 287.
Short and sweet this week. This article was too good to pass up, so please excuse the short TidBit Tuesday this week.
Safe fast to those of you observing Yom Kippur, Happy Feast of St. Francis of Assisi day and Happy Cinnamon Roll day to the rest of you! (Yes, that is actually a THING on October 4th.
Phenobarbital and Cats
It comes as no surprise that I'm a super fan of phenobarbital for seizure control in cats. My research at the University of Wisconsin started with the development of a novel transdermal phenobarbital product, and it ended (so far) with a novel oral formulation (not published yet). Phenobarbital works WELL and for many cats but, alas it isn't perfect.
Misconception vs. TRUTH
1) Phenobarbital causes elevated ALP enzymes in cats.....IT DOES NOT. There was one study that reported a few elevations but NONE of the 77 cats in a recent study, nor any of the cats in a prior study my resident and I conducted had elevated ALP enzymes. Elevated ALP is a dog thing!
2) Phenobarbital does not have observable side effects....FALSE! Side effects occur in 46.7%of cats (Marsh et al). Sedation and ataxia were the most common side effects, but not the only ones.
Here are the side effects (called Type A adverse events), and percent of cats affected, as reported in Marsh's study:
a. Sedation 89%
b. Ataxia 53%
c. Polyphagia 22%
d. Polydipsia 6%
e. Polyuria 6%
f. Anorexia 6%
** Perhaps the last 4 are only notable to the observant owner, or in single cat households. Also of note, side effects in cats are reported less often compared with dogs.
Type B adverse events were extremely rare in the recent study, as well as in my experience. Bone marrow suppression did occur in 1 cat (as can be seen with dogs) and it resolved with removal of the phenobarbital. Lymphadenopathy has been linked to phenobarbital use as well.
3) Phenobarbital side effects happen randomly...FALSE! They are dose dependent and predictable. Higher serum concentrations (above 35 ug/ml) result in a higher odds ratio of developing a side effect. Additionally, 20 of the 36 cats in the study by Marsh had transient signs. The majority of side effects only occured in the first 4 weeks of treatment. This is a terrific point to make when discussing the use of this drug with clients.
What is the Take Away Message?
1) Start phenobarbital at a dosage targeted to reach 20-30 ug/ml. This typically means about 3 mg/kg (or a bit less) q12h.The goal is seizure control without concerning side effects.
2) Counsel clients that side effects occur in about 1/2 of cats, and of those, the majority occur within the first 4 weeks of administration AND resolve without any dose adjustments. If side effects are present beyond 4 weeks, consider a dose reduction.
Happy Rosh Hashana to those celebrating and happy first day of Fall (a few days late)!
Keep those consults coming; I look forward to seeing you soon.
*Marsh O, Corsini G, Van Dijk J, Gutierrez-Quintana R, De Risio L. Prevalence and clinical characteristics of phenobarbitone-associated adverse effects in epileptic cats. Journal of Feline Medicine and Surgery. June 2020. doi:10.1177/1098612X20924925
*Finnerty K, Barnes Heller H, Mercier M, et al. Evaluation of therapeutic phenobarbital concentrations and application of a classification system for seizures in cats: 30 cases (2004 -2013). JAVMA 2014: 244(2):195-199.
Trazodone and the Neurologic Exam
Finally!! Trazodone and gabapentin are frquently recommended medications used for anxiolysis in the veterinary clinic but it has long been suspected that they have an impactful effect on the neurologic examination. We now have data! In this month's JVIM (https://doi.org/10.1111/jvim.16536), Drs. Lueck, Cameron and Zidan (from the University of Wisconsin-Madison!) evaluated 32 apparently healthy dogs pre and post trazodone administration and documented their findings.
Here are the key points:
1. The dose of trazodone in this study was 6.25-8.60 mg/kg PO single dose.
2. Neurologic examinations were performed before and 2.5 hours after trazodone administration
3. Decreased mentation changes were noted in about 25% of dogs (BAR going to QAR). Oddly enough, 7 dogs were noted to be QAR on initial exam and 3 were graded as BAR on post dosing exam. Not sure what to do with that except to say that we're obviously quite subjective on this assessment and BOTH are considered normal so should it matter?
4. Paw replacement deficits changed with identification of new, or worsened deficits in 22% of dogs. This finding isn't surprising but it bothers me. The neurologic examination is perhaps the most important tool to localize as well as determine differential diagnoses. We could misguide a client if we acted on the deficits identified while under the influence of trazodone!
5. Not a single dog had a worsening evaluation of their cranial nerves or reflexes in this study. Even 1 dog with reduced reflexes on the pre-trazodone assessment had similarly graded reflexes following trazodone administration.
What should we do with this information?
First, don't extrapolate to cats. Second, I strongly urge you not to have a client give trazodone to a pet prior to a neurologic examination based on this data. This recommendation has been previously based on my clinical suspicion so I'm thankful the authors went through the effort to perform and publish this data for the rest of us! Lastly, if you happen to do a neurologic examination on a pet ON trazodone and find deficits, consider repeating the examination without administration of trazodone to document consistence in the findings prior to recommending extensive work up. If that isn't possible, acknowledgement to the client of the possibility of a confounding factor, is recommended.
I look forward to hearing from you and working with you again soon! Have a great week and stay safe.
A cat with a tilt
Welcome! Today is a going to be a busy day! First on your case list is a sick cat so let's dive in. Here is the story:
The cat was presented for a 2-month history of a left head tilt. She was noted to have effusion from the left ear when signs started and was treated with amoxicillin (dose unknown) for 14 days. Clinical improvement was initially noted, but signs relapsed after medications were discontinued and now the owner's are noting a head tilt to the right, with wide head swinging movements (think Stevie Wonder) bilaterally, especially when she first wakes up. She is an indoor only cat, with a history of indoor-outdoor lifestyle over 5 years ago.
Physical Examination
General: T: 99.4 °F/37.4 C Pulse: 180 bpm Resp: 20 breaths/min
Wt.: 3.4 kg BCS: 4/9 MM
Eyes: Corneas are clear, no ocular discharge, normal conjunctiva.
Ears: Mild waxy debris noted in both external ear canals.
Oral cavity: Patient did not allow evaluation
Teeth: Did not evaluate.
Lymph nodes: Normal, no peripheral lymphadenopathy noted.
Heart: No murmurs or arrhythmias, pulses strong and synchronous.
Respiratory system: No nasal discharge, no tracheal sensitivity. Lungs clear on auscultation.
Abdomen: Normal, soft, non-painful, no masses or organomegaly noted.
Musculoskeletal: Not evaluated
Skin and hydration: dry flaky hair, no ectoparasites noted
NEUROLOGIC EXAMINATION
Palpation: No paraspinal pain elicited on palpation
Postural reactions: normal tactile placing and hopping all limbs.
Reflexes: Normal.
Gait: Ambulatory with mild vestibular ataxia and falling left.
Cranial nerve abnormalities: Wide head swinging with an occasional right AND left head tilt, positional rotary nystagmus, mild miosis OS, remainder normal.
Mentation: BAR, occasionally hissing
What is the neuronatomic lesion localization for THIS cat?
This cat has evidence of vestibular disease based on the presence of a head tilt and nystagmus. Cranial nerves 8 are affected by loss of function of the peripheral nerve, brainstem or cerebellum. To differentiate between these three localizations, it is important to evaluate the remaining neurologic examination for clues. Animals with brainstem disease will exhibit a loss of function of the upper motor neurons and ascending proprioceptive pathways which is demonstrated as evidence of ipsilateral hemiparesis and reduced ipsilateral proprioceptive testing. Furthermore, reduced level of alertness (obtunded, coma, stupor) may be noted. If paresis, proprioceptive deficits or reduced mentation are noted the lesion is most likely in the brainstem. Cerebellovestibular disease will manifest with signs of vestibular disease plus evidence of hypermetria, intention tremors and/or truncal sway, suggestive of cerebellar disease. Absence of these findings suggests a peripheral CN 8 neuroanatomic lesion localization. This cat does not have evidence of brainstem or cerebellar disease therefore the signs were localized to the peripheral component of CN 8.
Reduced sympathetic innervation to the eye may occur through damage to the sympathetic pathway. This pathway starts in the hypothalamus, courses caudally through the brainstem, cervical spinal cord, and exits the T1-T3 spinal cord segment and travels cranially in the jugular groove to the cranial cervical ganglion. From the cranial cervical ganglion this pathway runs through the middle ear and along the trigeminal nerve to end in the periorbital muscles, 3rd eyelid and dilator muscle of the iris. Dysfunction anywhere along this pathway will result in miosis in dim light. The lesion in this case is likely in the region of the middle ear due to a lack of neurologic disease noted in the intracranial structures, spinal cord, or along CN 5.
You may be tempted to call this a central lesion because the head tilts BOTH directions but don't! Without signs of hemiparesis, proprioceptive placing deficits or mentation changes a central lesion is unlikely.
Differential diagnoses: The history suggests that we now have a bilateral otitis media/interna but you couldn't rule out a polyp or neoplastic process with a secondary infection.
What did we do?
CBC and serum biochemistry were normal. Thoracic radiographs were unremarkable. The brain MRI showed bilateral debris in the bulla with ring enhancement.
Final diagnosis: Bilateral otitis media/interna. A myringotomy was performed, with ear flushing, cultures and cytology. Unfortunately no growth was noted (this is uncommon!) so marbofloxacin was started and clinical signs improved. She had a left head tilt on presentation for 30 day recheck, and this is expected to be permanent. All other signs of vestibular disease had resolved!
Happy first week of Fall everyone! I hope you and your family had a wonderful summer and look forward to working with you as we dig into what I hope will be a lovely Wisconsin fall.
Anisocoria in Dogs and Cats
** Credit for the amazing hand-drawn image goes to my good friend, and veterinarian Dr. Pam Boutilier.
Anisocoria
Anisocoria is defined as pupil asymmetry and may be seen with ocular or neurologic dysfunction. Malfunction of the sympathetic, parasympathetic, or visual system may result in anisocoria.
Neuroanatomy
Visual Pathway
When light enters the eye, it activates the light receptors in the retina. That information then travels along CN II, crosses in the optic chiasm, and terminates in the thalamus. Optic radiations relay the visual information from the thalamus to the visual cortex in the brain. This pathway can be tested using the menace response test and/or cotton ball testing.
Parasympathetic function: Pupil constriction
The parasympathetic pathway to the eye is a short, two neuron pathway which originates in the midbrain. The two, paired parasympathetic nuclei of CN III (PSNCNIII) send fibers along with the somatic nerves from CN III to the eye. The parasympathetic pathway is best assessed using PLR. When a bright light enters the eye, CN II activates and synapses on the PSNCNIII. The parasympathetic fibers transmit this information to the eye, using cranial nerve III as a conduit, resulting in pupillary constriction.
Sympathetic function: Pupil dilation
The opposing system is the sympathetic system, which causes pupillary dilation. The sympathetic pathway is a three neuron pathway and takes a longer course to the eye compared to the parasympathetic system. In general it goes from the thalamus, through the brainstem and cervical spinal cord to exit in the upper thoracic segments. Fibers then make a U turn and head back to the eye via the jugular groove (don't poke around too much when doing those jugular blood draws!), bulla (ear infection can = sympathetic dysfunction) and then hitches a ride with CN V to make the final leg to the eye. Malfunction anywhere along this pathway will result in a failure of iris dilation in a dark room and a comparatively miotic pupil, typically accompanied with enopthalmus and ptosis.
Putting it together
Let's put this new knowledge to work. If you see a case with anisocoria, how do you decide if it is a parasympathetic or sympathetic dysfunction?
1) Assess the pet in a dark room. Does the eye dilate? If yes --> The lesion is NOT due to sympathetic dysfunction.
2) Asses PLR. Does the eye constrict? If yes --> the lesion is NOT due to parasympathetic dysfunction.
To localize to the appropriate location beyond sympathetic or parasympathetic function requires a full neurologic examination. If you aren't comfortable performing or interpreting a neurologic examination please consider a neurology consultation! I am not comfortable doing a dental...we all have our limitations! :)
If you're interested in digging into anisocoria more deeply, or you have a case with anisocoria consider checking out the following article for a full discussion and more amazing images. Note: I do not receive any royalties or financial impact from this article.
* Barnes Heller H, Bentley E. The practitioner's guide to neurologic causes of canine anisocoria. Today's Veterinary Practice Jan/Feb 2016 pg. 77- 83.
Keep those consults coming; we all get to learn a little bit more with each consult. Have a great week!
Neutrophil-Lymphocyte Ratio in MUE
Meningoencephalomyelitis of unknown etiology (MUE) is a challenging antemortem diagnosis. MUE is the term used when we diagnosed inflammatory, non-infectious disease in the CNS. In the old days, we would have called this GME, NME or NLE, depending on the breed. However, those three inflammatory conditions cannot be distinguished on clinical picture, diagnostic testing, or treatment response, alone. Histopathology is needed to determine if a patient has GME, NME, and NLE. Without a brain biopsy, or post mortem sample, we cannot call it GME, NME or NLE. Several years ago, the term MUE started getting tossed around as an antemortem term for inflammatory brain disease, without a biopsy.
To diagnose MUE, a patient must have:
1) a neurologic examination with deficits identified (or a history of seizures) and
2) have a MRI with classical changes and
3) and CSF tap with a lymphocytic or monocytic pleocytosis and/or elevated protein level and
4) negative geographically specific infectious disease panel. If the pet meets these criteria, they can be diagnosed with MUE.
MUE does not show up in routine blood work. Inflammatory leukograms are rare, elevated body temperature is not typically reported and pets are not systemically, clinically ill. However, some immune mediated diseases (such as MS) have garnered attention for a neutrophil to lymphocyte ratio present on routine CBC.
A recent study out of Korea evaluated the ratio of neutrophils to lymphocytes in a standard CBC to see if we could predict a diagnosis of MUE. As it turns out, you can divide the neutrophil count by the lymphocyte count, and get a significantly higher number in dogs with MUE than healthy dogs. Furthermore, the ratio was significantly higher than dogs with idiopathic epilepsy but NOT different than dogs with brain tumors. The neutrophil-lymphocyte ratio was higher in dogs with MUE than all other forebrain diseases (hydrocephalus, idiopathic epilepsy, and brain tumors) but not always significantly so.
What does this mean for us?
Unfortunately, nothing...yet. This is an interesting concept and a step towards a much needed tool for diagnosing MUE without invasive diagnostic testing. Performing a CBC, and calculating the ratio, is both simple and readily available in most (all?) veterinary practices today. However, if the ratio is high, it does not mean the pet has MUE. It may support a diagnosis of forebrain disease (which you already know from your neuro exam) and may support structural brain disease (i.e. not idiopathic epilepsy). Very importantly - this study did not find a significant difference between dogs with brain tumors and those with MUE. Sadly, brain tumors and MUE are often our top differentials for pets with forebrain disease so this ratio does not (yet) give us another non-invasive tool to differentiate between these two diseases.
I enjoyed reading this study and learning about inflammatory markers for humans with MS (the human counterpart to MUE) and how this neutrophil-lymphocyte ratio could be used in the future for pets. If you'd like to read more, please see the link at the bottom of the page.
Thanks for reading! I hope you have a wonderful week and look forward to working with you soon!
If you haven't heard yet, please note that I am moving my office. Please try to remit any outstanding invoices by August 30th. If you need my new invoicing address please email me, or watch for a note in the mail.
Reference: https://onlinelibrary.wiley.com/doi/epdf/10.1111/jvim.16512
Ondansetron for Nausea in Vestibular Disease
Vestibular disease, whether it is central or peripheral in origin, can result in nausea and vomiting. The exact mechanism is unclear, but it is suspected to be via neuronal projections to higher centers (forebrain) and associated with activation of 5-HT3 receptors. Ondansetron is a selective 5-HT3 receptor antagonist (blocker). It has been shown to be effective on subjective observation, in controlling nausea in vestibular patients, but a recent double-blind placebo controlled study took it one step further. In addition to observation of signs of nausea, such as lip licking, facial expression, behavioral clues and hypersalivation, they evaluated blood levels of arginine vasopression (AVP) which has been positively correlated with nausea scores.
Materials and Methods
Eighteen dogs were enrolled, 14 were included in data analysis. Six dogs received placebo first, followed 2 hours later by ondansetron (0.5 mg/kg IV, diluted 1:1 with 0.9% saline). Eight dogs received ondansetron first, followed 2 hours later by placebo. Dogs were observed at hourly time points for signs of nausea (pre and post treatment) and had serum samples for AVP measurements taken at pre-treatment, 2 and 4 hours post initial treatment.
Key Results
Dogs given ondansetron, showed a rapid, significant reduction in nausea compared to dogs given placebo.
Only 4 dogs vomited, in addition to signs of nausea. ** Vomiting should not be the only sign you watch for to say a pet needs an anti-nausea medication!
Serum AVP concentrations decreased significantly after administration of ondansetron, compared to placebo.
Based on the data presented, it is reasonable to assume any dog with recent onset vestibular signs should be administered ondansetron if signs of nausea and/or vomiting are noted. It would be helpful to educate clients on the signs of nausea (not just refusing food or vomiting!) when performing at-home observation of their pets with vestibular disease.
Interested in learning more about the nausea scores? Please consider this reference:
1. Kenward H. Development of an objective means of assessing nausea in dogs. London:EThOS British Library; 2015.
I hope you're doing well and look forward to working with you soon!
Reference for article discussed above: 0.1111/jvim.16504
Walk This Way: Describing Ataxia and Paresis in the Clinical Patient
Perhaps you’ve wondered what the difference is between ataxia and paresis? Perhaps you already know, in which case you can grab that cup of coffee and move on to your next email!
Still with me? Okay, here we go. Ataxia is the failure of coordination. This suggests a sensory abnormality and when noted, it is a hallmark for neurologic disease. As you’ll see in the next section, paresis can be noted with neurologic, orthopedic, neuromuscular or muscular conditions, making it much less specific. Ataxia, however, is a failure of neurologic sensory information which means it can only be noted with dysfunction of the neurologic system. There are three forms of ataxia: 1) proprioceptive, 2) vestibular and 3) cerebellar.
Proprioceptive ataxia is an indication of a spinal cord, brainstem or forebrain disease. Ataxia is not noted with neuromuscular disease. Signs of proprioceptive ataxia include a crossing of the limbs when walking down a straight pathway, or placing the limbs narrow and wide of the midline of the body without regularity.
Vestibular ataxia indicates dysfunction of the vestibular apparatus. When observing a patient with vestibular ataxia, the observer can appreciate a falling or drifting towards one side when walking. This can be especially magnified when the patient is turned in a circle.
Cerebellar ataxia occurs with disease or injury to the cerebellum. Signs of hypermetria, truncal sway, and a wide based stance with, or without intention tremor are indications of cerebellar ataxia.
Paresis, on the other hand, is a weak movement or incomplete paralysis. This involves most commonly UMN or LMN, but remember the neuromuscular junction, muscle and bones or joints can be a source of paresis also. A patient with mild paresis will exhibit a reduced joint range of motion when walking giving the appearance of shuffling. Severe paresis may be more profound so that an animal is unable to support weight even with purposeful limb movements.
Common terminology when describing paresis:
Mono: one limb (any)
Para: pelvic limbs (both)
Tetra: four limbs
How can you write the gait abnormality in the record?
If the pet has only a proprioceptive ataxia: Pet is exhibiting crossing of pelvic limbs, consistent with proprioceptive ataxia.
If the pet has proprioceptive ataxia AND paresis: Pet shows crossing of pelvic limbs and reduced joint ROM (or weakness /unable to rise/collapsing frequently) consistent with proprioceptive ataxia and paraparesis.
If the pet is non-ambulatory in the pelvic limbs (cannot walk without support): non-ambulatory paraparesis*
If the pet does not have any observable motor, even with support, in the pelvic limbs: paraplegia. *
*Comments about ataxia cannot be made once the pet is non-ambulatory or plegic.
Hopefully this helps clarify when to use paresis and ataxia when describing the gait. Enjoy your week and stay safe!
Book Announcement!
Small Animal Neuroanatomic Lesion Localization Practice Book
Over the last 18 months I have been collaborating with many amazing neurologists across the globe to write a first ever Neuroanatomic Lesion Localization Practice Book and.... IT'S ALMOST HERE!
I received confirmation recently that they expect to have this baby in the warehouse by November 2022! Self promotion is hard, so hopefully the book will speak for itself.
If you feel the need to brush up on your lesion localization technique, or are entering an internship or residency soon and want to get a jump on the neuroanatomic lesion localization game, or maybe you know a soon-to-be veterinary student that might benefit from this little ditty - you're in luck! Here is the link if you wish to check it out. (http://www.cabidigitallibrary.org/doi/) The book is titled: Small Animal Neuroanatomic Lesion Localization Practice Book. Let me know if you have any questions!
And now...back to the grind. :)
Thanks for reading! I hope you have a good week and stay cool out there in this heat.
Intervertebral Disc Herniation in Cats
Intervertebral disc herniation (IVDH) does occur in cats but is reported at a much lower prevalence than dogs. Is this because the disease is less prevalent or because owners are less likely to pursue advanced diagnostic imaging to obtain a diagnosis? I don't know the answer, however a recently published article reported on 35 cases of feline TL IVDH over 21 years. That sounds like a lot fewer cases than we see for dogs!
Clinical Presentation
Like dogs, the most common presenting complaint is difficulty walking and/or pain. In this study, They found 2 cats had grade I, 20 cats were grade II, 7 cats were grade III, 3 cats were grade IV and 3 cats were grade V on presentation. (Grading scale listed at the bottom). There was no significant difference between outcome at discharge or follow up and initial presenting grade. Does that mean that we shouldn't rush to get cat's seen, imaged, and cut? Probably not. Of the 3 grade V cats (the ones that we would consider a surgical emergency), one improved, one was static and the other was lost to follow-up. What was the timeline for surgery? Unknown. Dogs have a 50% chance of improvement if they are grade V and undergo surgery within 24 hours. This is debated amongst neurosurgeons but as a general rule I subscribe to the plan of cut ASAP whenever possible if deep pain is absent.
Location of the Offending Disc
In the referenced study, thoracolumbar disc herniation was most common at L6-7. This is slightly different from the previous reports in which L7-S1 was reported to be most common, but not far off. I think it is safe to say that cats are more likely to have low lumbar disc herniation than T11-L2 disc herniation, like dogs. Why? Cats are SO MUCH more flexible than most dogs (especially the chondrodystrophic type) that the vertebral dynamics are different as well. Previous reports suggest obesity is more common in cats with IVDH (and in my experience, too) but this cannot be the entire answer. It remains to be seen, why cats are more likely to have a low lumbar disc herniation than TL. When someone knows...I'll tell you!
Key Points:
Intervertebral disc herniation does occur in cats
The most common presenting sign is weakness or lumbar pain
Surgery can be done and SHOULD be done (when appropriate for the patient)
If you have a cat patient with lumbar or lumbosacral pain, reach out. I'd love to see them! Schedule a consult using my online scheduler (for veterinary use only) and let's get your patients feeling better, soon!
Grading scale:
Grade I: normal gait with hyperpathia
Grade II: ambulatory paraparesis
Grade III: non-ambulatory paraparesis
Grade IV: paraplegia with intact nociception
Grade V: paraplegia with absent nociception
Reference: https://journals.sagepub.com/doi/pdf/10.1177/1098612X211028031